Mutant flu paper is finally published, reveals pandemic potential of wild viruses
It’s finally out. After months of will-they-won’t they and should-they-shouldn’t-they deliberations, Nature has finally published a paper about a mutant strain of bird flu that can spread between mammals.
The strain was produced by Yoshihiro Kawaoka from the University of Wisconsin-Madison, who was trying to understand whether wild bird flu viruses have the potential to start a pandemic. These viruses can occasionally infect humans, but so far, they’ve been contained by their inability to efficiently jump from human to human. Kawaoka’s work makes it clear that they can evolve that ability.
Kawaoka’s study, along with a similar one from Ron Fouchier, has been the subject of intense debate for the last several months (catch up on the backstory here). What are the benefits of the research, and do they outweigh the risks? Now that the paper is finally out, we can start to answer those questions.
I’ve written about the paper for Nature News, focusing very heavily on the science rather than the politics. Head over there for a tighter version of this story. In this post, I’m going to highlight four important themes from the paper.
One: H5N1 can evolve to spread between mammals with worrying ease
This work was never about creating strains of killer viruses. It was always about uncovering what the wild viruses could potentially do. To understand how, you need to know exactly what Kawaoka did.
To begin an infection, flu viruses stick to receptor proteins on the surface of their host cells, known as sialyl glycans. Bird flu viruses prefer to stick to a version of these receptors called Siaα-2,3, found in bird cells. Human flu viruses prefer to stick to the Siaα-2,6 type that dominate our upper airways. This difference explains why most bird flu viruses have a tough time infecting humans.
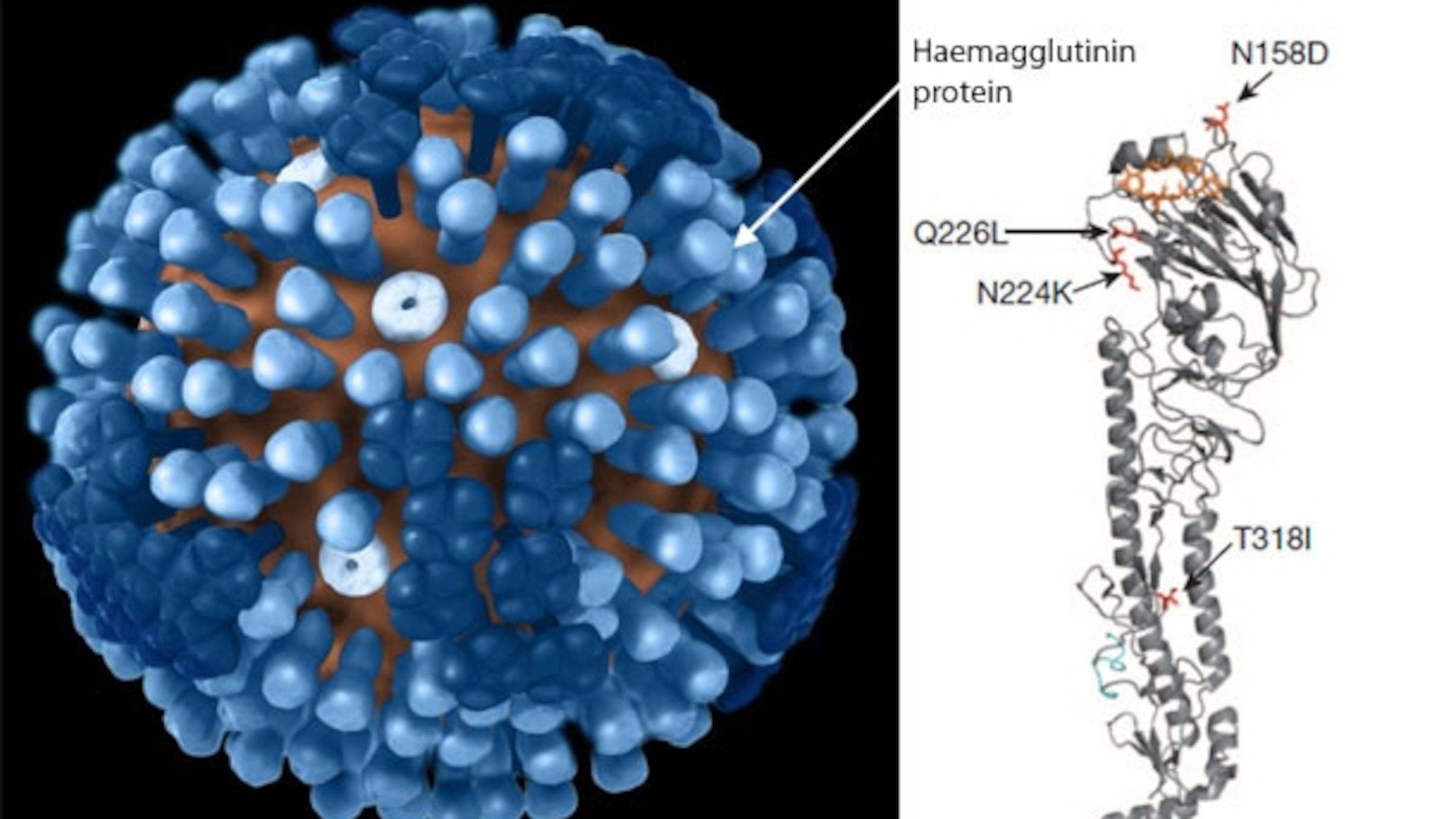
To see if bird flu could evolve to recognise the human-type receptors, Kawaoka mutated the haemagglutinin protein (HA), which allows the virus to stick to its hosts. HA dots the surface of the virus like pins in a cushion. Kawaoka randomly introduced mutations into the head of the pin. Of the millions of mutants he created, just one stuck to the human-type receptors over the bird ones. Just two mutations conferred this ability – N224K and Q226L.
Next, Kawaoka fused this mutated HA with seven other genes from the H1N1 virus that caused a pandemic in 2009 – you probably know it as “swine flu”. In the wild, viruses often swap (or ‘reassort’) their genes in this way, so Kawaoka’s hybrid virus is one that could emerge naturally.
The virus could successfully infect ferrets – the animal that best simulates a flu infection in humans. One of the ferrets shed particularly high levels of virus from its nose. When Kawaoka sequenced these viruses, he found that they had naturally evolved a third mutation – N158D.
He then applied this three-mutation virus to six ferrets, and housed them next to six healthy animals. After a week, the virus had spread to four of the uninfected ferrets, and along the way, it had picked up a fourth mutation – T318I – which made it even more transmissible. When Kawaoka tested this four-mutation strain on six more ferrets, they transmitted it to all six of their healthy partners.
The mutant strain can spread between ferrets, but it does so less effectively than the pandemic strain that swept the world a few years back. It causes less severe disease than that strain or wild H5N1, and it didn’t kill any of the ferrets. And it’s vulnerable to both Tamiflu, and a prototype H5N1 vaccine.
That’s good news. But it’s more worrying to think about what actually happened in the experiments. Kawaoka’s active efforts to mutate the HA protein only led to the first two mutations. At this point, the virus could recognise mammal cells but couldn’t spread through the air. It evolved that ability on its own, in just two rounds of infection in ferrets. Kawaoka started the process, but the ferrets completed it. Sophisticated genetic techniques couldn’t produce a virus that spread between mammals. Evolution did it in a few generations. Go figure.
Jeremy Farrar, who studies flu viruses in Vietnam, says, “After the cynicism that arose in some quarters following the 2009 pandemic, this work reminds us just how vulnerable we potentially are to relatively small changes.”
Two: There appear to be two traits that make for a transmissible virus – specificity and stability.
Three of the mutations – N224K, Q226L, and N158D – sit in the head region of HA and allow it to recognise human-type receptors. We always knew that the viruses need this ability to infect humans, so this isn’t particularly new.
It’s the fourth mutation that’s interesting. T318D sits in the stalk of the protein, and serves to stabilise it, compensating for problems that the other three cause.
One a flu virus binds to the surface of its host cell, it is swallowed up. Once inside, the acidic conditions within the cell trigger a change in the shape of the HA protein. This transformation allows the virus to fuse with the cell, and release its genetic material. This is a critical step – without it, the virus cannot make copies of itself.
The three mutations that allow the virus to recognise human-type receptors screw up the timing of these events. Because of them, the HA protein undergoes its transformation in less acidic surroundings, which means that it often does so before it gets into a cell. That’s bad news for the virus, because the change is irreversible. If it happens outside a cell, the virus is basically a dud. Kawaoka thinks that the T318D stabilises the HA protein so, as before, it only changes shape inside a cell. Now, it can recognise a mammalian cell and reproduce properly inside it.
The point about stability is new. Wendy Barclay from Imperial College says, “With hindsight it makes perfect sense.” However, it’s not a property that scientists had focused on before.
Three: It’s not the mutations that matter, but what they do. Or, don’t miss the wood for the trees.
Critics might argue that knowing about these four mutations tells us very little, for three reasons. First, ferrets aren’t humans, and the same mutations might not allow H5N1 to spread between us. Second, Kawaoka’s virus was a hybrid, so we don’t know if a pure H5N1 virus with these four mutations would behave in the same way. Third, there could be hundreds of other mutations that produce the same effects. This is especially true for the stabilising mutations. HA’s stability is determined by its entire structure, so mutations in any part of the protein could potentially do the same job as T318I.
These are valid points, but they are also red herrings. The value of this study is not in identifying four specific mutations, but in identifying what they do. Kawaoka thinks that in the field, scientists might sequence wild viruses to look at these specific mutations. That’s the genotype. But it would be more valuable to look for the traits that they confer – specific and stability. That’s the phenotype.
To check for specificity, scientists could test viruses to see if they recognise human-type receptors. To check for stability, they could simply heat the viruses to 50 degrees Celsius. Normal H5N1 and the version with just two HA mutations lose their infective powers at this temperature, but the four-mutation version keeps on going. These are simple tests, and they may be important for assessing the pandemic potential of naturally occurring viruses.
The same principles may apply to other types of flu besides H5N1. For example, Daniel Perez found that a hybrid H3N2-H9N2 virus could also evolve to spread between mammals with two mutations – one involved in specificity and one involve in stability.
Four: Wild viruses are almost there.
This is the important bit. Some wild viruses already have many of the necessary components to spread from mammal to mammal. There are strains in Egypt that can bind to human-type receptors. The N158D mutation is found in the wild. And there are wild viruses with mutations in other important genes, such as PB2, that allow them to reproduce efficiently in humans.
Maybe some of these viruses are a stabilising mutation away from… well, going viral. In the movie Contagion, Laurence Fishburne’s character says, “Someone doesn’t need to weaponise the bird flu. The birds are doing that.” The line was spot on.
Some might argue that Kawaoka’s virus is a hybrid, and a pure H5N1 virus might behave differently. This isn’t an objection that provides much comfort. H5N1 and pandemic H1N1 are found in many of the same parts of the worlds. They have both been recovered in pigs. And their genes are highly compatible. Not all flu viruses can swap genes effectively, and H5N1 produces weak, inviable viruses when it merges with some seasonal flu strains. However, it hybridises very well with the pandemic H1N1. This means that Kawaoka’s hybrid virus is a very real possibility rather than some sort of fictitious, far-fetched creation.
For several months, people have worried about experiments that artificially produced more transmissible strains of flu. Yes, this research has genuine risks, but the point is that similar experiments are already going on all around us – in the tissues of wild birds, pigs, and other animals. They’re the ones to worry about, and they don’t require regulatory approval. The lab experiments could help us to understand how the natural ones are going to play out.
Reference: Imai, Watanabe, Hatta, Das, Ozawa, Shinya, Zhong, Hanson, Katsura, Watanabe, Li, Kawakami, Yamada, Kisos, Suzuki, Maher, Neumann & Kawaoka. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature http://dx.doi.org/10.1038/nature10831
Image by Doug Jordan, from the CDC, combined with figure from Imai et al.
More on flu:
- Why did a US advisory board reverse its stance on publishing mutant flu papers?
- Mutant flu – the risks and benefits
- Building anti-flu drugs on a computer
- A crystal ball for predicting the future of flu
- How drug-resistant flu took us by surprise
- Flu viruses take the summer off to go travelling
- Flu and Parkinson’s – how H5N1 bird flu causes neural degeneration in mice
- From Spanish to swine – how H1N1 kicked off a 91-year pandemic era
- Origins of the swine flu pandemic
- Flu survivors still immune after 90 years
- Round peg, square hole – why our bird flu drugs are a fluke
- New flu viruses emerge in tropical Asia before going on one-way world tour
Go Further
Animals
- Octopuses have a lot of secrets. Can you guess 8 of them?
- Animals
- Feature
Octopuses have a lot of secrets. Can you guess 8 of them? - This biologist and her rescue dog help protect bears in the AndesThis biologist and her rescue dog help protect bears in the Andes
- An octopus invited this writer into her tank—and her secret worldAn octopus invited this writer into her tank—and her secret world
- Peace-loving bonobos are more aggressive than we thoughtPeace-loving bonobos are more aggressive than we thought
Environment
- Listen to 30 years of climate change transformed into haunting musicListen to 30 years of climate change transformed into haunting music
- This ancient society tried to stop El Niño—with child sacrificeThis ancient society tried to stop El Niño—with child sacrifice
- U.S. plans to clean its drinking water. What does that mean?U.S. plans to clean its drinking water. What does that mean?
- Food systems: supporting the triangle of food security, Video Story
- Paid Content
Food systems: supporting the triangle of food security - Will we ever solve the mystery of the Mima mounds?Will we ever solve the mystery of the Mima mounds?
History & Culture
- Strange clues in a Maya temple reveal a fiery political dramaStrange clues in a Maya temple reveal a fiery political drama
- How technology is revealing secrets in these ancient scrollsHow technology is revealing secrets in these ancient scrolls
- Pilgrimages aren’t just spiritual anymore. They’re a workout.Pilgrimages aren’t just spiritual anymore. They’re a workout.
- This ancient society tried to stop El Niño—with child sacrificeThis ancient society tried to stop El Niño—with child sacrifice
- This ancient cure was just revived in a lab. Does it work?This ancient cure was just revived in a lab. Does it work?
Science
- The unexpected health benefits of Ozempic and MounjaroThe unexpected health benefits of Ozempic and Mounjaro
- Do you have an inner monologue? Here’s what it reveals about you.Do you have an inner monologue? Here’s what it reveals about you.
- Jupiter’s volcanic moon Io has been erupting for billions of yearsJupiter’s volcanic moon Io has been erupting for billions of years
- This 80-foot-long sea monster was the killer whale of its timeThis 80-foot-long sea monster was the killer whale of its time
Travel
- How to plan an epic summer trip to a national parkHow to plan an epic summer trip to a national park
- This town is the Alps' first European Capital of CultureThis town is the Alps' first European Capital of Culture
- This royal city lies in the shadow of Kuala LumpurThis royal city lies in the shadow of Kuala Lumpur
- This author tells the story of crypto-trading Mongolian nomadsThis author tells the story of crypto-trading Mongolian nomads